Over the past month, the Territory has seen a remarkable and alarming increase in COVID-19 cases. While there are breakthrough cases among the vaccinated and even the vaccinated and boosted, evidence continues to show that the risk of severe illness, hospitalization, and death are significantly decreased in the vaccinated and boosted population.
One of the critical factors in this new wave is the presumed presence of the Omicron variant in the Territory. New information about the Omicron variant has led the CDC, and the Government of the Virgin Islands, to issue new guidance. In this post we’ll review updated masking protocols, updated quarantine guidance, and updated regulations and resources in the Territory.
Masks
One of the most important facts about the Omicron variant is its transmissibility– it spreads at least three times faster than the Delta variant. One infectious COVID positive person can be expected to infect three other people, on average. In an article by NPR, Dr. Robert Wachter, chair of the Department of Medicine at the University of California, San Francisco, says “It’s very contagious, and the kind of encounter that you could have had with prior versions of the virus that would have left you uninfected, there’s now a good chance that you will get infected from it.”
Preliminary data suggests that patients infected with the Omicron variant may expel more virus particles than patients infected with earlier variants, and that those virus particles may linger in the air in indoor environments for much longer than earlier variants. For these reasons, cloth masks that have served many people well until this point may no longer provide adequate protection.
Experts recommend that you upgrade your mask to a high-filtration option like N95, KN95, or KF94 respirator masks. These are all made out of material with an electrostatic charge, which actually pulls virus particles in and prevents you from inhaling them. Surgical masks also have an electrostatic charge, but their looser fit makes them less effective against something as infectious as the Omicron variant.
When considering when to wear your mask, it’s best to err on the side of caution. It remains important (and often mandated) to wear a mask on public transit and in indoor public spaces. However, it may also be wise to mask up when gathering indoors with small groups of family and friends outside of your social bubble, unless everyone is vaccinated and boosted. This is especially important if anyone attending is considered high risk.
Quarantine
You have likely heard that the Centers for Disease Control and Prevention (CDC) updated their guidelines on quarantine and isolation on Monday, December 27th.
Per the new recommendations:
- The recommended time for isolation for people with COVID-19, IF ASYMPTOMATIC, is shortened from 10 days to 5 days, followed by 5 days of masking around others.
- Therefore, people who test positive should isolate for 5 days and, if asymptomatic at that time, they may leave isolation if they can continue to mask for 5 days to minimize the risk of infecting others.
- You should continue to isolate as long as you are symptomatic.
- If you know that you have been exposed to a COVID positive case, the quarantine requirement has been updated as well
- If you are unvaccinated or more than six months out from an mRNA vaccine (or more than two months out from the Johnson & Johnson vaccine) and not yet boosted, the CDC recommends quarantine for five days followed by strict mask wearing for five more days.
- Individuals who have been vaccinated and boosted do not need to quarantine, but should adhere to a strict mask-wearing policy for the next ten days, ensuring that their mask is well-fitting.
- For all those exposed, the best practice is to test for COVID-19 at day five after exposure.
- All GVI agency heads are authorized to allow government workers who can work remotely to do so from December 28th, 2021 until January 10th, 2022. In-person services during this period will be limited. Please be patient and understanding as you go about your business.
- Bar, restaurants, and nightclubs are ordered closed at midnight, and the last call for alcohol will be 11 pm. This will continue until January 10th, 2022.
- Planned Crucian Christmas Festival events on January 4th, 5th, and 6th are cancelled.
- Beginning on Monday, January 3rd, ALL travelers into the Territory will be required to submit a negative test taken within 72 hours prior to travel, whether vaccinated or not, including persons vaccinated in the USVI.

With the holiday season in full swing, people are gathering together again to reconnect with loved ones. However, data suggests another spike in cases of COVID-19 is likely. Extra precautions are still needed to slow the spread of the virus and its more contagious variants. With that in mind, we’ve pulled together some tips for a safer holiday season.
Incorporate as many layers of protection as possible at your holiday gatherings to keep all of your attendees safe. Consider the following options:
- Keep things small, especially if you invite seniors or people who are immunocompromised.
- Celebrate outdoors, or socially distanced indoors, to lower the chance of transmission.
- Have conversations with others about their vaccination status before you see them, and set boundaries ahead of time.
- Get a flu shot. The CDC estimates that flu shots in the U.S. reduce the risk of illness for 40-60% of the population.

On Tuesday, July 27th, the Centers for Disease Control and Prevention released new guidance regarding mask wearing, as the delta variant of COVID-19 spurred a surge in cases nationwide. Here in the U.S. Virgin Islands, we have seen a significant increase in our positivity rate over the past two weeks as a result of the delta variant, and our neighbors in the British Virgin Islands are experience a devastating wave of cases.
In May, the CDC announced that fully vaccinated individuals did not need to wear a mask outdoors or indoors in most situations. While the mask mandate never changed in the U.S. Virgin Islands, the new guidance is a significant shift for many in the United States.
Specifically, the new recommendations state that people who live where coronavirus transmission is classified as substantial or high should wear masks when they are indoors in public places, whether they are vaccinated or not. In addition, the guidance calls for universal mask-wearing in K-12 schools, including teachers, other staff members, students and visitors. This recommendation applies to everyone over the age of 2.
The new guidance is largely a result of the delta variant of COVID-19, which is responsible for the majority of new cases in the United States, and has been confirmed present in the U.S. Virgin Islands. The delta variant is more highly transmissible than earlier iterations of the virus, and new research, not yet published, suggests that fully vaccinated people who have breakthrough infections may have similar viral loads to unvaccinated people who become infected. The increased likelihood that vaccinated people with breakthrough infections can spread the virus is the main reason the mask guidance has been updated.
Masks continue to be an important intervention for people at heightened risk of severe illness from COVID-19 because of a weakened immune system, an underlying medical condition or advanced age.
So, where and when should you be wearing a mask? If you’re vaccinated, check the CDC case tracking for your local area. If the positivity rate is significant or high, you should be wearing a mask in public indoor spaces, and likely in crowded outdoor spaces as well. All staff and students in schools should be wearing masks. If you’re unvaccinated, you should continue to wear a mask in public and practice social distancing.

Last Friday, April 23rd, the Centers for Disease Control and Prevention (CDC) issued a Johnson & Johnson vaccine update when they voted to end the pause on its use. That vote paved the way for the Food and Drug Administration (FDA) to officially end its recommended pause as well. Therefore, this week the nation will see states and territories resume use of the single-dose Covid-19 vaccine.
Moving forward, the FDA will include a warning on the J&J packaging which notes the potential risk of rare blood clots. This warning reflects the events that triggered the vaccine’s pause last week, when reports emerged of a rare clotting disorder in six women who received the J&J vaccine. Since then, nine more cases have emerged, all in women.
In their announcement on Friday the FDA released updated fact sheets on the vaccine, and noted that most of those who developed the rare clots were women between the ages of 18 and 49. They also stated that the “chance of having this occur is very rare”. To date there have been seven cases reported per million doses given among women in that age group.
“Safety is our top priority. This pause was an example of our extensive safety monitoring working as they were designed to work—identifying even these small number of cases. We’ve lifted the pause based on the FDA and CDC’s review of all available data and in consultation with medical experts and based on recommendations from the CDC’s Advisory Committee on Immunization Practices. We have concluded that the known and potential benefits of the Janssen COVID-19 Vaccine outweigh its known and potential risks in individuals 18 years of age and older. We are confident that this vaccine continues to meet our standards for safety, effectiveness and quality. We recommend people with questions about which vaccine is right for them have those discussions with their health care provider,” – Janet Woodcock, M.D., Acting FDA Commissioner.While news like this can be alarming, this pause and investigation into the emerging reports is actually reassuring. It indicates that the system used to monitor vaccine safety is working as intended. Nearly eight million doses of the J&J vaccine have been administered so far. Among men and women 50 or older, there has been less than one case reported per million doses administered. In addition to being a single-dose vaccine, the Johnson & Johnson shot is easier to store than the two dose versions from Moderna and Pfizer. Therefore, the vaccine is especially useful when providing equitable access to homebound, homeless, and incarcerated populations, as well as remote communities. Here in the U.S.V.I. the Johnson & Johnson vaccine is being prioritized for homebound residents. Appointments can be made through the Virgin Islands Department of Health As always, you should speak to your primary care provider before getting the vaccine if you have any underlying conditions. Specifically, the FDA recommends you speak to your physician if you:
- Have allergies
- Have a fever
- Have a bleeding disorder or are taking blood thinners
- Are immunocompromised or are taking a medicine that affects your immune system
- Are pregnant or planning to become pregnant
- Are breastfeeding
- Have received another Covid-19 vaccine
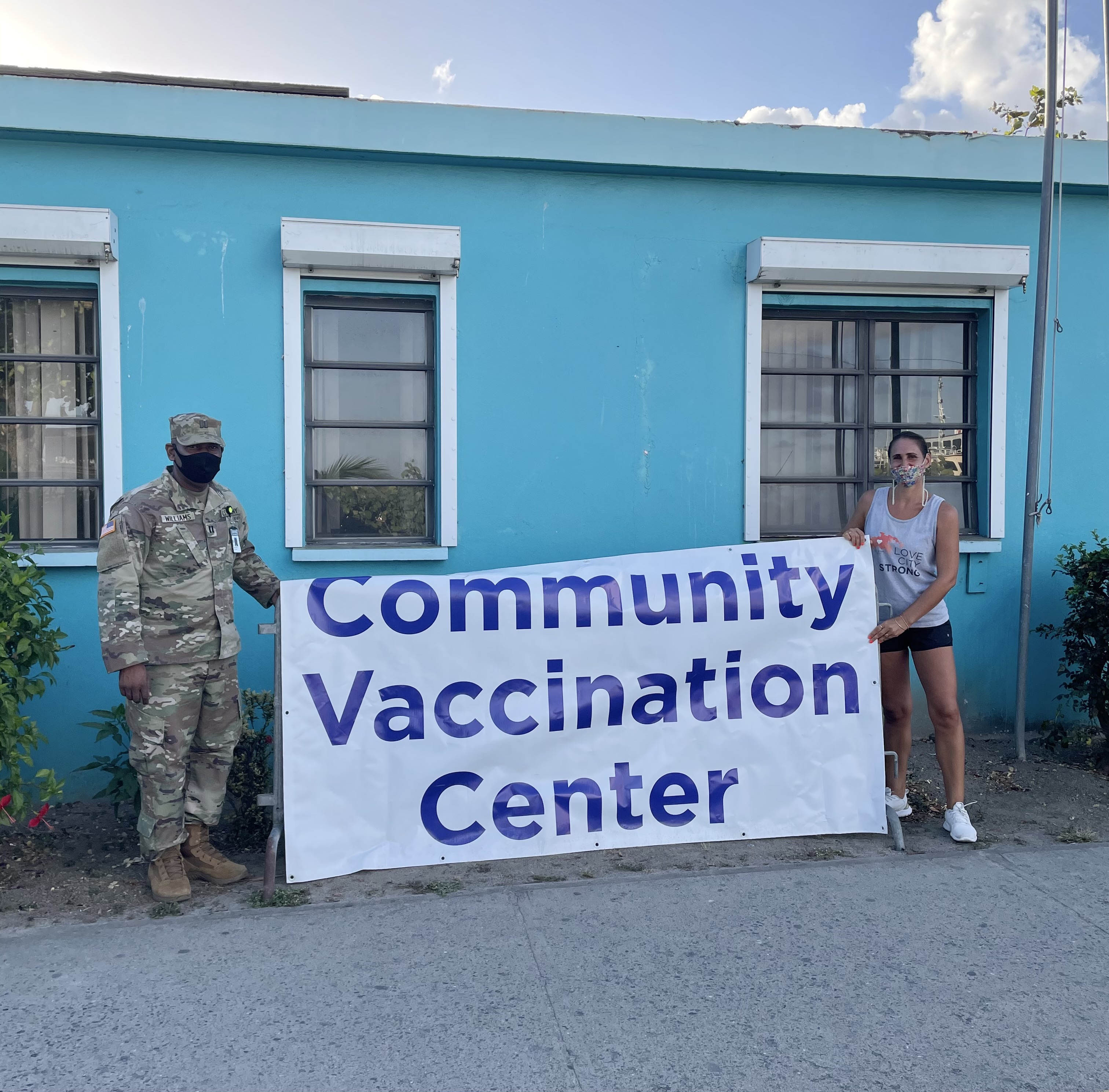
As the COVID-19 pandemic has progressed, we have made every effort to meet the moment in terms of our response to the ever-changing circumstances. Our team’s connection to the community, along with forward thinking to potential hazards and challenges, has allowed us to respond quickly and efficiently throughout this crisis. To that end, as 2020 drew to a close we began preparing ourselves to assist the Territory with COVID-19 vaccination efforts on St. John.
In November, we began reaching out to contacts in the healthcare field to get a better understanding of the COVID-19 vaccines that were being developed. Through short training sessions we were able to educate ourselves about the vaccines, and about vaccinations in general. We purchased additional PPE and secured donations from Good 360 to help the healthcare community prepare for the inevitable surge in PPE use that would result from any sort of mass-vaccination effort in the Territory.
In January 2021, we developed messaging and content related to the vaccines across a variety of channels. We wanted to ensure that we could start debunking myths, providing facts, and answering questions about the vaccines as soon as possible to increase vaccine confidence in the St. John community.
In February our team was vaccinated by the Island Health and Wellness Center, with our employees who are seniors or licensed emergency first receiving their doses first. We then began the process of collecting data from individuals across the island to help shape our outreach efforts. We spoke to over 500 St. John residents and asked them questions about whether they had received or planned on receiving the vaccine, along with additional demographic questions. Using this data we crafted specific messaging to reach certain segments of the community via phone calls and home visits to help answer questions and provide information from the VI Department of Health.
In March, we were asked to assist in the mass-vaccination efforts on St. John. For the last five weeks we have partnered with the VI Department of Health, VITEMA, the Virgin Islands National Guard, the CDC, and the United States Department of Defense in running vaccination pop up clinics in Cruz Bay every Saturday. Our supplies, manpower, and knowledge of the community have been utilized to make vaccination efforts on St. John more robust.
We have provided tables, chairs, PPE, and bottled water for staff and patients at every pop up. Our Go Team has done extensive outreach directly to residents’ homes to sign them up for future appointments, and picked up seniors and individuals with limited mobility to bring them to their appointments. We have also provided Spanish speaking translators and logistical assistance to the pop ups as needed.
The trust of our donors has given us access to a significant amount of unrestricted funds, enabling us to meet immediate needs. Unrestricted funding is extremely important to the work that we do so that we do not have to hesitate to respond when an emergency happens. To support our vaccination efforts, and our efforts to prepare for the future, click here.
To learn more about the COVID-19 vaccine, visit the VI Department of Health’s resource page; the CDC’s Vaccine FAQ page, and the Johns Hopkins guide for fully vaccinated individuals. You can also check out our vaccine Q&A with Sandy Colasacco, a Board Certified Family Nurse Practitioner and the Clinical Executive Director of Island Health and Wellness.

As COVID-19 vaccination efforts continue in the US Virgin Islands and across the globe, many are wondering what to expect when they receive their doses, or are trying to decide if they should get vaccinated in the first place.
We interviewed members of our team who have received the vaccine, and asked them to share a little bit about their experience before and after receiving it.
Kenisha Small, our Community Relations Manager (pictured above, left) and Deborah Ramsay of our Go Team (pictured above, right) were both vaccinated at the Island Health and Wellness Center on St. John in February.
Here’s what they had to say (responses have been edited for length and clarity):
Why did you choose to get the vaccine?
Deborah: I got the vaccine for three reasons: The work I do directly helping and speaking with St. John seniors; because my doctor advised that, since I am over 65, the possible side effects of the vaccine were likely much less severe than the side effects of getting COVID; and because my daughter and family said they would not want me traveling to visit them in the United States if I chose not to get the vaccine.
Kenisha: I got the vaccine to assist in keeping the seniors in my family and our community safe.
Did you have any fears or anxieties about getting the vaccine?
D: Yes! I am fairly anti-vaccine. I have never gotten a flu shot, for instance. I was concerned about the side effects and was unsure about how effective (the vaccine) might be.
K: I was more surprised at the fact that they had already created a vaccine for something so seemingly new.
What were some of the resources that you found helpful in answering questions about the vaccine? In other words, where or who did you turn to for information?
D: My daughter, the internet, friends, colleagues, and my doctor.
K: I turned to my coworkers at LCS for guidance and gaining knowledge to build my confidence; specifically our Operations Manager Stephen, who is also an EMT and our Executive Director, Meaghan.
Describe your experience getting the vaccine.
D: I went to Island Health & Wellness. We had to wait outside the office briefly. Once inside, there was a lot of paperwork to fill out. We were kept at a safe distance from each other. It took about 1/2 hour including filling out the paperwork and having to sit in the office for 15 minutes after getting the shot to observe us for possible immediate side effects. The shot took seconds and was hardly noticeable! And I HATE shots. They scare me and I can’t watch. But it happened so quickly I barely noticed!
K: I got an appointment at 2pm for the vaccine at Island Health and Wellness. The entire process took about 45 minutes to an hour, which included arriving early, waiting in line, and remaining for 15 minutes after receiving the shot. Process was simple, somewhat smooth and quick once inside.
Which vaccine did you get?
D: Pfizer
K: Pfizer. I’ve had my first dose and am due to receive the second dose on March 4th.
Did you experience any side-effects after your vaccine doses?
D: Yes. A slightly sore arm for a few days. The first night, it was hard to sleep on that side. After the first shot I felt a little sick that night and most of the next day. I had slight body aches, a bit of a headache, and low energy. After the second one, (I had) slightly less effects. Mostly just low energy.
K: I had a sore arm for a few days, and on the day of the shot I just felt lazy or sluggish afterwards; otherwise it went well!
What’s one thing you think that everyone getting the vaccine should know?
D: The shot itself is barely noticeable. At Island Health, they were very efficient. Plan to rest the day after!
K: From what I can tell, it’s safe!
For more information about the COVID-19 vaccine, check out the Virgin Islands Department of Health’s FAQ page, the CDC’s vaccine information website, and this video from Johns Hopkins Medicine.

This week, our team partnered with the Virgin Islands Fire Department and Our Lady of Mt. Carmel Catholic Church to help distribute boxes of food to St. John residents as part of the USDA’s Farmers to Families program.
While this is the fourth time that boxes of food have been given out on St. John, the current distribution model relies on those in need going to distribution sites.
Our team’s inclusion in this round of distribution ensured that a crucial group of individuals was able to receive this program’s benefits: Seniors and people with a disability or chronic health condition that renders them homebound. We delivered boxes of food directly to 80 homes across the island in a single day.
Our longstanding model of going directly to those we serve for all of our programs, rather than making them come to us, means that we are uniquely able to navigate St. John quickly and efficiently. This allows us to provide people with goods and services from other organizations who might otherwise not be able to access them.
Thanks to the support of our Board and donors, we are able to provide vehicles for our employees to participate in programs like this. Providing our team with vehicles, PPE, and the tools that they need to do their jobs ensures that they do not have to use their personal property for work purposes. This lends itself to our belief in a strong work-life balance, and strengthens our impact.
Your donations ensure that we can continue to support other organizations’ efforts when we are not working on our own programs. Click here to read more about what we do, and please consider a donation today. With your help, we can keep supporting our community whenever we are able.
As the COVID-19 vaccines continue to roll out around the world, there’s a lot to learn. Among other things, experts continue to make the case for social distancing protocols even after you’re vaccinated. This may seem counterintuitive, but there are important reasons to listen to their recommendations. Traditional public health safety protocols will continue to be important day to day.
You’ve gotten your second dose of the COVID-19 vaccine… now what?
Congratulations! It may be tempting to throw caution to the wind after a year of living carefully, but the time is still not right. Based on the guidance of the CDC, you should continue following all COVID-19 safety protocols. Yes, that means even after you’ve been vaccinated, at least for a while longer.
Why is this important?
The vaccine roll out is making significant progress in many places. However, we have not yet achieved a level that provides herd immunity. Therefore, the unvaccinated portions of the population are still vulnerable. Additionally, while the vaccines do protect the recipient from more severe cases of COVID-19, they may not fully prevent the vaccine recipient from passing the virus along. In other words, while the vaccine protects you, it may not make you less of a risk to unvaccinated or immunocompromised people.
What should I do?
The good news is, it’s simple to stay responsible!
- Continue wearing a mask when you’re in public or around people who are not in your COVID pod.
- Maintain six feet of social distance whenever possible.
- Wash your hands regularly and thoroughly.
- Continue to avoid large gatherings, particularly indoors.
In December of 2019 the world was introduced to the 2019 novel coronavirus (2019-nCov), now commonly known as COVID-19.
Scientists worldwide immediately began to map the genome of the virus. This means they were essentially learning the blueprint of how it’s built and how it works. Genome mapping is the first step to understanding a virus and learning how to treat it.
As the COVID-19 pandemic worsened, the development of a vaccine became a global priority. Experts around the world shifted to a single focus, and ultimately yielded the fastest vaccine development in history.
As with any new-to-market vaccine or treatment, people have questions. Are these vaccines safe? Are they effective? What are the long term effects? All of these questions and more are valid. Access to accurate scientific facts and data is helpful in understanding the COVID-19 vaccines.
The two vaccines that are currently available in the United States (at the time of this post’s publication) are the Pfizer vaccine and the Moderna vaccine. Both of these fall into the category of mRNA vaccines. Different types of vaccines work in different ways, but their purpose is always the same – teach your body to recognize an intruding illness and defend itself against the intruder.
Today’s COVID-19 messenger RNA (mRNA) vaccines are based on more than 30 years of research. This type of vaccine is of particular interest because they can be developed in a laboratory using readily available materials, making them easily standardized and scalable compared to more traditional vaccination techniques. For these reasons, development can move more quickly once the virus’ genome has been mapped.
Messenger RNA vaccines have been studied in the past for flu, Zika, and rabies. Cancer research has used mRNA to trigger the immune system to target specific cancer cells. In the future, scientists hope that mRNA vaccine technology can use one vaccine to target multiple diseases, thereby reducing the overall number of vaccinations that a person needs.
Some important facts about the COVID-19 mRNA vaccines include:
- mRNA vaccines do not use the live virus that causes COVID-19.
- mRNA never enters the nucleus of the cell, which is where our DNA (genetic material) is stored.
- The cell breaks down and gets rid of the mRNA soon after it is finished using the instructions.

December 7th is the start of National Influenza Vaccination Week (NIVW). NIVW is an annual observance reminding everyone age 6 months and older that there’s still time to get vaccinated and #FightFlu in your community.
Flu vaccinations are more critical than ever this year as COVID-19 continues to spread at alarming rates. Combating both viruses has already placed a tremendous burden on healthcare systems around the globe. This may result in many more illnesses, hospitalizations and deaths than during a typical flu season.
Even for those who are young, healthy, and have no preexisting conditions, getting a flu vaccine is still important. By getting vaccinated we prevent ourselves from becoming vectors of disease and causing undue harm to others.
The CDC estimates that flu vaccinations in the U.S. reduce the risk of illness for 40-60% of the overall population. In other words, the more people who vaccinate in a community, the more that their community is protected.
Do your part to protect your community by getting your annual flu vaccination. Flu vaccinations are a simple act that has the potential to save lives, support our healthcare workers, and make a real difference.
Visit www.GetMyFluShot.org to learn more.
For a partial list of vaccination providers in your area, click here.
To learn more about the similarities and differences between the influenza virus and COVID-19, check out this video from Johns Hopkins Medicine.